Staff Nurse Exam Question Answers- April 2018 ESIC Staff Nurse Exam Model Question Answers-2019
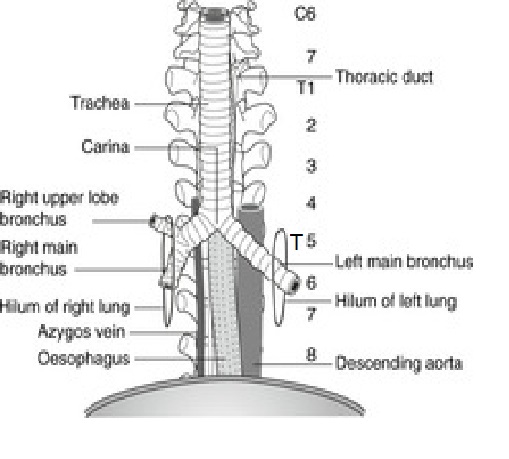
1. Before endotracheal intubation some facts about trachea a nurse has to understand and all the following are true regarding trachea except
- It is about 13 cm long
- It bifurcates into two major bronchi
- It starts at te level of 7th cervical vertebra
- It ends at the level of sternal angle of Louis
2. Contraindication for expectant regime in placenta praevia are all except
- Bleeding at 36 wks
- Profuse bleeding
- Baby dead
- Congenital anomaly of foetus
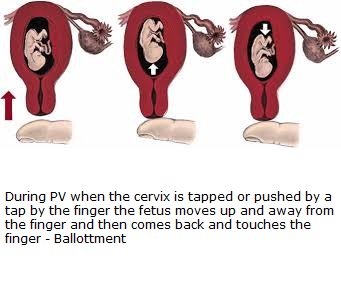
3. Active foetal movement felt by the mother is
- Quickening
- Lightening
- Ballotment
- Softening
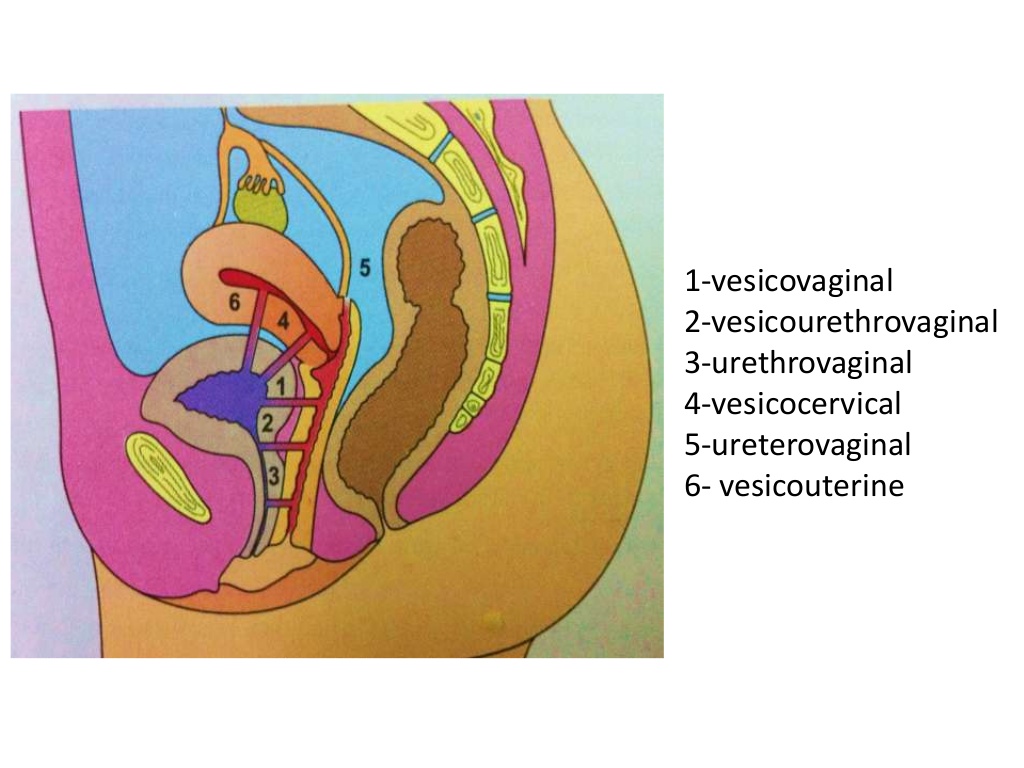
4. Commonest type of Genito urinary fistulae
- Vescico vaginal
- Utero vaginal
- Vescico uterine
- Urethro vaginal
5. Mr. Mukthar Ahamad is undergoing chest physiotherapy after CABG. Which of the following levels of prevention it illustrates?
- Primordial
- Primary
- Secondary
- Tertiary
6. Lower esophageal sphincter tone is high in
- Achalasia Cardia
- Diffuse Esophageal Spasm
- Nut Cracker Esophagus
- Ineffective Esophageal motility
7. Puberty menorrhagia is managed by
- Danazol
- Progestogens
- Oestrogens
- D&C
8. Contraceptive failure is calculated by
- Pearl Index
- Pincus Index
- Russel Index
- Reids Index
9. Commonest malignancy of maxillary sinus is
- Squmous cell carcinoma
- Adeno carcinoma
- Adenoid cystic carcinoma
- Rhabdomyosarcoma
10.Most common post operative psychiatric condition is
- Depression
- Schizophrenia
- Mania
- Delirium
11. Electro convulsive therapy was first introduced by
- Moniz and Lima
- Cerletti and Bini
- Fraud and Jung
- Meduna and Paracelsus
12. The following are true about retraction except
- Muscle fibres permanently shortened
- Progressive and intense during 1st stage
- Special property of upper uterine segment
- Effects haemostasis after separation of placenta
13. Delusion is a disorder of
- Perception
- Thought
- Orientation
- Memory
14. Simpson grading is used to assess the completeness of surgical removal of
- Gliomas
- Meningiomas
- Pituitary adenomas
- Vestibular schwannomas
15. Cardiac failure is most likely in pregnancy at
- 32 Wks
- 1st Stage of labour
- III Stage of labour
- D:-4th Stage of labour
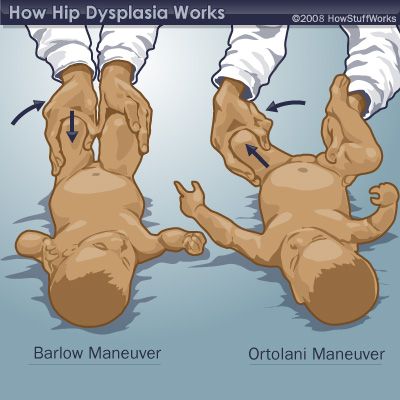
16. The test used to detect hip instability is
- Barlow's test
- Weber test
- Phalan test
- Alen test
17. The commonest gynaecological cause of retention urine
- Vaginal operations
- Ovarian tumours
- Cervical fibroid
- Haemato colpos
18. Softening of cervix during pregnancy is
- Osiander's sign
- Goodell's sign
- Chadwick's sign
- Chvostek's sign
19. Commonest false localizing sign in raised intracranial pressure is
- Oculomotor nerve palsy
- Abducent nerve palsy
- Facial nerve palsy
- Papilloedema
20. A patient treated for infertility with clomiphene presents with sudden onset of abdominal pain and distension
with ascites. Probable cause is
- Uterine rupture
- Ectopic pregnancy
- Multi fetal pregnancy
- Hyper stimulation syndrome
21. A group of related ideas or statements is called
- theory
- conceptual framework
- philosophy
- paradigm
22. Bleeding in the first trimester with no uterine contraction or pain and dilatation of cervix indicates
- Threatened abortion
- Complete abortion
- missed abortion
- inevitable abortion
23. Bacillus cereus food poisoning is commonly associated with the consumption of
- green beans
- fried rice
- Bottled honey
- Baked potato
24. A scale that cannot be used to assess a subject for a mood disorder is
- Edinburgh inventory
- Hamilton rating scale
- Wakefield questionnaire
- Beck inventory
25. when there is a possibility of locked twins being born ?
- First twin has cephalic and the second twin has breech presentation
- Fraternal twins
- First twin has breech and the second twin has cephalic presentation
- Dichorionic diamniotic twins
26. An immovable joint is called
- Synarthrosis
- Amphiarthrosis
- Diarthrosis
- Polyarthritis
27. In the diagnostic atatement "Excess fluid volume related to decreased venous return as manifested by lower extremity edema (swelling ) " the etiolog of the problem is :
- Edema
- Excess fluid volume
- Decreased venous return
- Idiopathic
28. Which of the below is NOT a function of the fibrous skeleton of the heart?
- Forms a structural foundation for the heart valves
- Conducts the impulses from atria to ventricles
- Prevents overstretching of the valves
- Acts as a point of insertion for cardiac muscle fibres
29. The microorganism that is usually a part of the normal vaginal flora but can cause meningitis in newborns is :
- Candida albicans
- Group B streptococci
- Staphylococcus epidermidis
- Corynebacterium species
30. Proton pump in stomach is an example for :
- Simple diffusion
- Facilitated diffusion
- Secondary active gransport
- Primary active transport
31. Voluntary rejection of unacceptable thoughts or feeelings from conscious awareness is called :
- Substitution
- sublimation
- Symbolisation
- Suppression
32. The professional value of nursing that describes the right toself-determination is called :
- Integrity
- Autonomy
- Dignity
- Altruism
33. Which of the following is NOT a part of the secondary prevention of mental illness ?
- Early detection
- Rehabilitation
- Crisis stabilisation
- Screening
34. Introduction of solid foods along with brreast feeding is called
- Scheduled feeding
- Demand feeding
- Complementary feeding
- Conditional feeding
35. Pseudo hyphae are seen in :
- Penicillium
- Aspergillus
- Candida
- Mucor
36. Naegele's rule is used to calculate :
- Amniotic fluid
- Cervical dilatation
- Gestational age
- Expected date of delivery
37. The test that is most specific for myocardial damage is:
- Myoglobin
- Troponin I
- Creatinine kinase
- CK-mb
38. The first level in the healthcare system is:
- Secondary health care
- Primary health care
- Primordial health care
- Tertiary health care
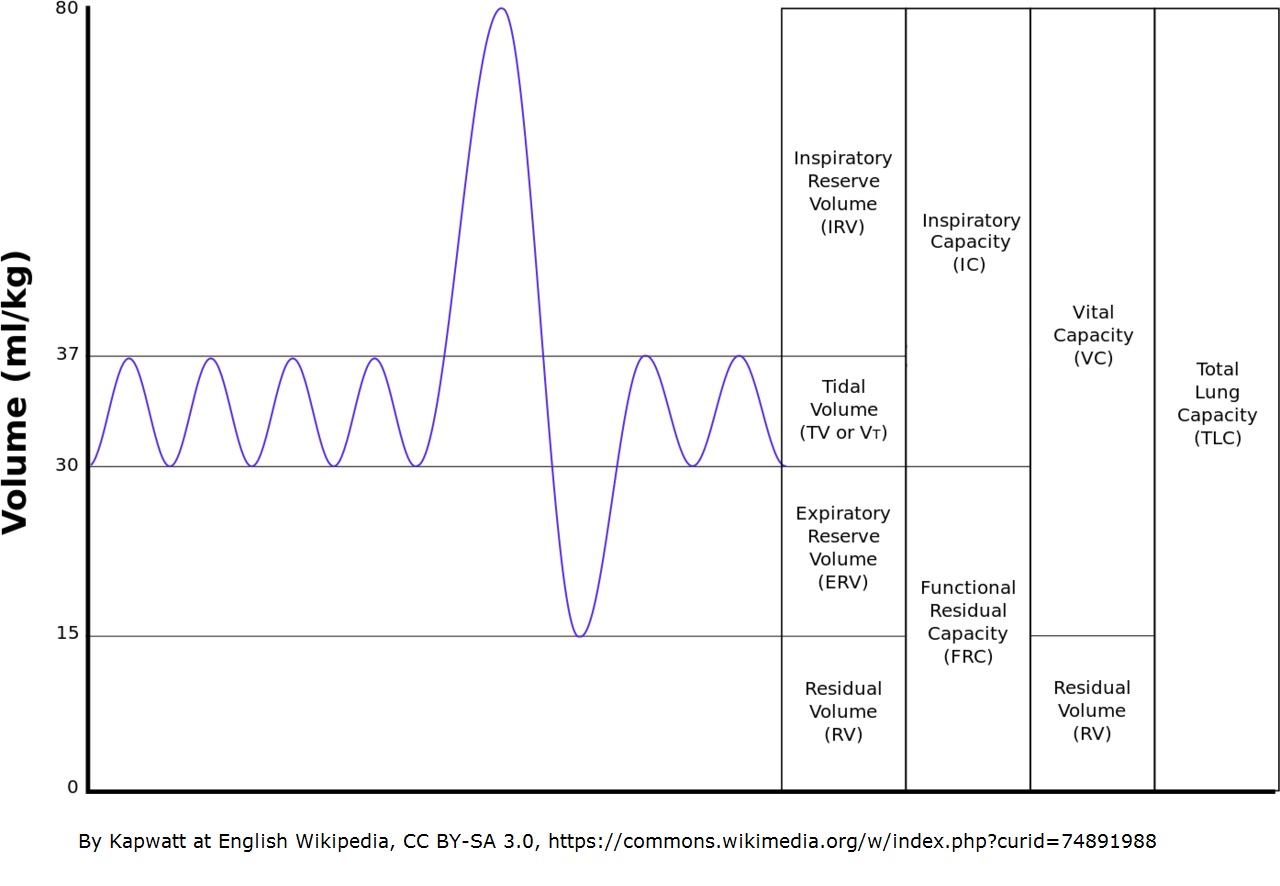
39. Respiratory rate multiplied by tidal volume gives :
- Total lung capacity
- Maximum voluntary ventilation
- Minute volume
- Expiratory reserve volume
40. Fine downy hair, normally found abundantly in premature babies, is called :
- Vernix
- Lanugo
- Caput
- Naevi
41. In a patient taking high doses of acetaminophen over a prolonged period, the parameter tob e monitored regularly is:
- Kidney function
- Liver function
- GI irritation
- Prothrombin time
42. Depolarisation in a nerve action potential is due to :
- Opening of potassium channels
- opening of calcium channels
- Opening of sodium channels
- Closing of sodium channels
43. The action of the sympathetic system in the walls of airways is called :
- Bronchodilatation
- Increased gas exchange
- Bronchoconstriction
- Increased secretion
44. Which of the following is true with regards to pregnancy-induced hypertension ?
- There is raised BP before 20 weeks' gestation
- Proteinuria is usually present
- It is also called as gestationalhypertension
- Visual disturbances are always present
45. The most common cause of retinal detachment is:
- Degenerative changes in the retina or vitreous
- Brain tumors
- Trauma
- Diabetes mellitus
46. The term MRSA in bacteriology stands for:
- Multidrug Resistant Staphylococcus aureus
- Methicillin Resistant Streptococcus anginosus
- Methicillin Reactive Staphylococcus aureus
- Methicillin Resistant Staphylococcus aureus
47. The document that gives nurses the authority to carr out specific actions under certain circumstances, often when a physician is not immediately available, is called :
- Discharge summary
- Standing order
- Prescription
- Concept map
48. The genera that needs pyridoxal for growth is:
- Granulicatella
- Pedi coccus
- Aero coccus
- Enterococcus
49. Which surgical procedure has the highest incidence of ureteric injury ?
- vaginal hysterectomy
- werthimes hysterectomy
- abdominal hysterectomy
- anterior colporrhaphy
50. Normal intracranial pressure in adults is
- 1-7 mm Hg
- 7-15 mm Hg
- 15-25 mm Hg
- 20-30 mm Hg
51. Which type of hallucinations are common in schizophrenia ?
- Olfactory
- Tactile
- Auditory
- Visual
52. Puberty menorrhagia is managed by
- Danazol
- Progestogens
- Oestrogens
- D & C
53. Tincture of iodine is :
- Alcoholic solution of Iodine
- Solution of Iodine in aqueous KI
- Aqueous solution of Iodine
- Aqueous solution of KI
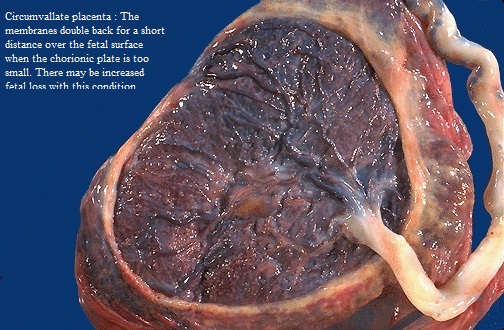
54. A thin fibrous ring present at the margin of the chorionic plate is:
- Placenta marginata
- Placenta circumvallate
- Placenta succentrata
- velamentous insertion
55. All of the following are included in electromagnetic spectrum except
- Visible light
- gamma rays
- Beta rays
- X-rays
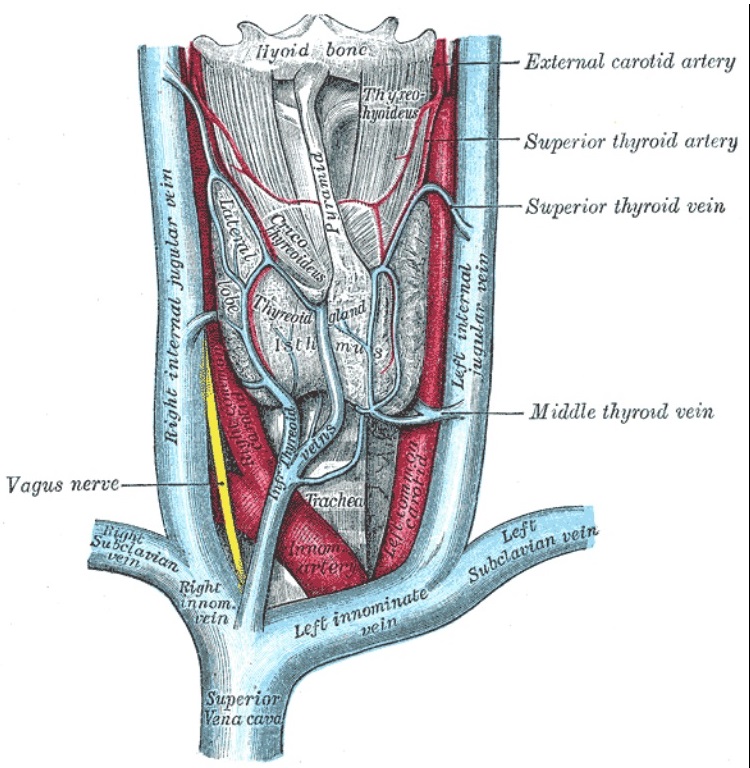
56. External jugular vein drains into which ofthe following vein :
- Facial vein
- Brachiocephalic vein
- Subclavian vein
- Internal jugular vein
57. Contraceptive failure is calculated by
- Russel index
- Pincus index
- Pearl index
- Reids index
58. Normal serum bilirubin level is
- 1-2 mg %
- 0.1 - 0.7 mg%
- 0.2 - 0.8 mg%
- 0.4 - 1.2mg %
59. In a normal average infant, how much more will be the growth of body length compared to the body length at birth ?
- 20 %
- 50 %
- 75%
- 10 %
60. Which of the following is NOT assimilated by eukaryotic cells ?
- Lactate
- Nitrogen
- Glucose
- Sulphate
61. An unattractive man selects expensive , stylish clothes to draw attention to himself. The defense mechanism exemplified here is :
- Compensation
- Conversion
- Denial
- Dissociation
62. Which of the following is the mortality indicator ?
- Prevalence rate
- Crude death rate
- Incidence rate
- Morbidity rate
63. Neuroleptic drugs are also known as :
- Hypnotics
- Antiepileptics
- antidepressants
- Antipsychotics
64. When a person's blood pressure drops, the kidneys respond by :
- Secreting renin
- Increasing urine output
- Slowing the release of ADH
- Producing aldosterone
65. Which is NOT a high risk factor that might affect workers in a construction company ?
- Traumatic injuries
- Allergic diseases
- Malnutrition
- Chest disease
66. The normal order of events taking place during thesecond stage of labour is :
- Descent → flexion → crowning → extension → internal rotation
- descent → flexion → internal rotation → extension → crowning
- Descent → internal rotation → crowning → extension → flexion
- Descent → flexion → internal rotation → crowning → extension
67. Which of the following is NOT a component of HELLP syndrome ?
- Bleeding pervaginum
- Low platelet count
- Elevated liver enzymes
- Hemolysis
68. Poor skin turgor in neonates and infants indicates :
- Hypoglycemia
- Hypertonia
- Dehydration
- Hypocalcemia
69. Which of the following is NOT a sign of respiratory distress ?
- Nasal flaring
- Changing of posture to ease breathing
- Speaking complete sentences
- Cyanosis
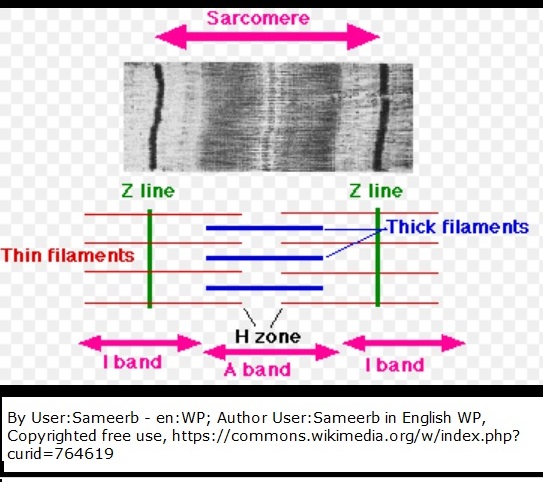
70. Which of the following is the true statement about the H zone of the sarcomere ?
- It contains thin filaments only
- It contains thick filaments only
- It is devoid of thck or thin filaments
- It contains thick and thin filaments lying side by side
71. Srub typhus is caused by :
- Rickettsia prowazekii
- Orientia tsutsugamushi
- Rickettsia akari
- Rickettsia typhi
72. Which of the following is a confirmed indication of pregnancy ?
- Nausea and vomiting
- Amennorrhea
- Fetal heart in ultra-sonogram
- Beta HCG in urine
73. The minimally invasive technique by which thin, insulated lead wire with electrodes (neurostimulator) is surgically implanted in the brain is called :
- Functional MRI
- Transcranial magnetic stimulation
- Deep brain stimulation
- Electroconvulsive therapy
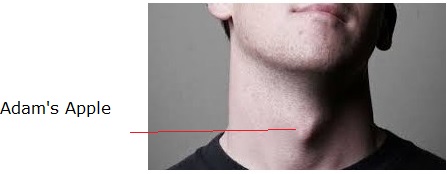
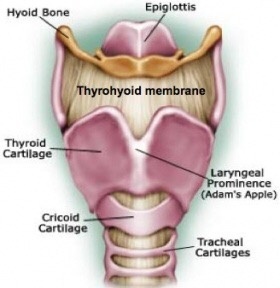
74. The "Adam's Apple " is formed by :
- Hyoid bone
- Thyroid cartilage
- Epiglottis
- Cricoid cartilage
75. The meaning of remission is :
- the person is clinically cured
- the severity of disease increases
- The disease is present, but the person does not experience symptoms
- The symptoms reappear
76. Lactational amenorrhoea acts as a contraceptive method by :
- Preventing implantation
- Preventing ovulation
- Preventing sprem entry
- Spermicidal action
77. The test used for the diagnosis of trichomoniasis is :
- Specific serologic test
- Ova and parasite fecal smear
- Enzyme-linked immunoassay (ELISA) test of serum
- Wet mount of vaginal fluid
78. The third phase of body's adaptation to stress is :
- Resistance
- Exhaustion
- Rebound
- Reaction
79. . Tuberculosis is caused by polluted:
Air
Water
Food
Fomites.
80. Polio is transmitted through:
- Water
- Air
- Food
- Insects
81. A person with no sign of disease but may transmit, it is called:
- A resistant person
- Immune person
- A carrier person
- An allergic person.
82. For eye examination the instrument used is:
- Stethoscope
- Otoscope
- Opthalmoscope
- Percussion hammer
83. Thyroid gland is present in:
- Chest
- Abdomen
- Neck
- Back
84. Who is regarded as “Father of Medicine”?
- Paracelsus
- Aristotle
- Galen
- Hippocrates
85. Dehydration is caused in the human body due to:
- Less of vitamins
- Loss of water
- Loss of Salt
- Loss of minerals.
86. All these are sterilized by chemicals except:
- Scissors
- Endoscopes
- Gauze
- Cables
87. B.C.G. vaccine is given to protect the child against:
- Diphtheria
- Tetanus
- Typhoid
- Tuberculosis
88. Protein deficiency disease is known as:
- Kwashiorkar
- Cushing’s disease
- Gaucher’s disease
- None of these above
89. Bone deformation can occur due to lack of:
- Calcium
- Phosphorus
- Vitamin D
- All of these
90. Vitamin ‘D’ deficiency may result in:
- Rickets
- Beriberi
- Scurvey
- Night blindness
91. Which is not cancer:
- Leukaemia
- Glaucoma
- Carcinoma
- Sarcoma
92. Vitamin essential for coagulation of blood is:
- B
- D
- K
- A
The Question Paper with Answer of ESIC Staff Nurse Examination conducted on 26/02/2019 and 27/02/2019 is published on 03/03/2019. Nurse Examination conducted on 26/02/2019 and 27/02/2019 is published on 03/03/2019.
In the first decades of the 18th century in the Dutch Republic, Daniel Gabriel Fahrenheit[7] made two revolutionary breakthroughs in the history of thermometry. He invented the mercury-in-glass thermometer (first widely used, accurate, practical thermometer)[2][1] and Fahrenheit scale (first standardized temperature scale to be widely used).[2]
In 1714, Dutch[7] scientist and inventor Daniel Gabriel Fahrenheit invented the first reliable thermometer, using mercury instead of alcohol and water mixtures. In 1724, he proposed a temperature scale which now (slightly adjusted) bears his name. He could do this because he manufactured thermometers, using mercury (which has a high coefficient of expansion) for the first time, and the quality of his production could provide a finer scale and greater reproducibility, leading to its general adoption. In 1742, Anders Celsius (1701–1744) proposed a scale with zero at the boiling point and 100 degrees at the freezing point of water,[17] though the scale which now bears his name has them the other way around.[18
Era of precision thermometry
See also: Precision thermometry, Fahrenheit scale, Celsius scale, Mercury-in-glass thermometer (mercury thermometer), Medical thermometer, Clinical thermometer, Pyrometer, and Infrared thermometer
Daniel Gabriel Fahrenheit, the originator of the era of precision thermometry.[14] He invented the mercury-in-glass thermometer (first widely used, accurate, practical thermometer)[1][15][16] and Fahrenheit scale (first standardized temperature scale to be widely used).
A medical mercury-in-glass maximum thermometer.
In 1714, Dutch[7] scientist and inventor Daniel Gabriel Fahrenheit invented the first reliable thermometer, using mercury instead of alcohol and water mixtures. In 1724, he proposed a temperature scale which now (slightly adjusted) bears his name. He could do this because he manufactured thermometers, using mercury (which has a high coefficient of expansion) for the first time, and the quality of his production could provide a finer scale and greater reproducibility, leading to its general adoption. In 1742, Anders Celsius (1701–1744) proposed a scale with zero at the boiling point and 100 degrees at the freezing point of water,[17] though the scale which now bears his name has them the other way around.[18] French entomologist René Antoine Ferchault de Réaumur invented an alcohol thermometer and, temperature scale in 1730, that ultimately proved to be less reliable than Fahrenheit's mercury thermometer.
The first physician to use thermometer measurements in clinical practice was Herman Boerhaave (1668–1738).[19] In 1866, Sir Thomas Clifford Allbutt (1836–1925) invented a clinical thermometer that produced a body temperature reading in five minutes as opposed to twenty.[20] In 1999, Dr. Francesco Pompei of the Exergen Corporation introduced the world's first temporal artery thermometer, a non-invasive temperature sensor which scans the forehead in about two seconds and provides a medically accurate body temperature.[21][22]
Abstract
The human placenta is a villous hemochorial structure. It is attached to the uterine wall and establishes connection between the mother and the fetus through the umbilical cord and thus plays a critical role in maternal fetal transfer. It is developed from two sources: fetal chorion frondosum and maternal decidua basalis. Various abnormal conditions have been reported with the placenta and the placental chorioangioma is one of them. Chorioangioma of placenta is the commonest benign tumor of the placenta. It consists of a benign angioma arising from the chorionic tissue. It has been found to be associated with many serious complications such as nonimmune hydrops, congenital abnormalities, hemolytic anemia, polyhydramnios, IUGR, and IUFD.
Keywords
chorioangiomafetusplacentapolyhydramniosvilli
Chapter and author infoShow +
1. Introduction
The human placenta is discoid in shape and is a villous hemochorial structure [1, 2]. The placenta is attached to the uterine wall and establishes connection between the mother and the fetus through the umbilical cord and thus plays a critical role in maternal fetal transfer [2]. It has a complex synthetic capacity and plays a role in the immunologic acceptance of fetal allograft [2].
2. Development
The placenta is developed from two sources. The principal component is fetal which develops from the chorion frondosum, and the maternal component consists of decidua basalis (Figure 1) [2]. The fertilized ovum converts into a morula and further differentiates into a blastocyst. The outer layer of the blastocyst proliferates to form the primary trophoblastic cell mass which infiltrates the endometrial lining. By the 7th post-ovulatory day, the trophoblast differentiates into two layers: an inner layer of clear mononuclear cells with well-defined limiting membranes called cytotrophoblast and the outer layer of multinucleated cells with no intercellular membrane called syncytiotrophoblasts [1]. By 10th to 13th post-ovulatory days, a series of intercommunicating spaces or lacunae develop in the rapidly enlarging and dividing trophoblastic cell mass.
Figure 1.
Decidual structure differentiating into decidua basalis, capsularis, and parietalis.
The lacunae become confluent, and as the trophoblastic cell erodes the maternal vessels, they become filled with blood to form intervillous spaces. Between the lacunae spaces, there are columns having a central core of cytotrophoblasts surrounded by syncytiotrophoblasts. These form the framework for the development of villi later. From these pillars, branching sprouts appear. Those columns extent as far as the decidua and a mesenchymal core develops in them to form extraembryonic mesenchyme, which forms the villus vessels. In due course, these vessels establish continuity with those developing from the body stalk and inner chorionic mesenchyme. The distal part of the columns is not invaded by the mesenchyme but only serves to anchor it to the basal plate [1, 3]. These cells proliferate and spread laterally separating the syncytiotrophoblasts into two layers, the definitive syncytium on the fetal aspect and the peripheral syncytium on the decidual side which eventually degenerates and is replaced by a fibrinoid material and is known as Nitabuch’s layer.
With deeper blastocyst invasion into the decidua, the extravillous cytotrophoblasts give rise to solid primary villi composed of a cytotrophoblast core covered by syncytium. The most deeply implanted portion of these villi forms placenta (Figure 2). Beginning on the 12th day after fertilization, chorionic villi can first be distinguished and form secondary villi. After angiogenesis begins in the mesenchymal cores, it results into tertiary villi.
Figure 2.
Development of placenta.
By approximately the 17th day, fetal blood vessels are functional, and a placental circulation is established. The placenta is a vascularized villus structure by the 21st day. The fetal-placental circulation is completed when embryonic blood vessels are connected with chorionic vessels. Groups of cytotrophoblasts also grow into the lumen of the spiral arteries extending as far as the decidual myometrial junction. These cells destroy the muscular and the elastic layer of the vessel wall and get replaced by a fibrinoid material which is derived from the maternal blood and proteins secreted by the trophoblastic cells. This primary invasion dilates the spiral arteriolar wall and thus augments blood flow to the placenta [1, 3]. There is a secondary invasion of trophoblast between 12 and 16 weeks extending up to radial arteries within the myometrium. Thus, spiral arteries are converted to large bore uteroplacental arteries. The net effect is funneling of the arteries that reduce the pressure of the blood to 70–80 mm Hg before it reaches the intervillous space. It thus increases the blood flow.
The placental septa appear by 12 weeks protruding into the intervillous spaces from the basal plate and divide the placenta into 15–20 lobes. Until the end of the 16th week, the placenta grows both in thickness and circumference due to growth of the chorionic villi with accompanying expansion of the intervillous space and with continuous arborization and formation of fresh villi [2].
In the first trimester, the villi are large and have a mantle of trophoblasts consisting of an inner layer of cytotrophoblasts and an outer layer of syncytiotrophoblasts with the stroma of small fetal vessels. During the second trimester, the villi are smaller, the mantle is less regular and the cytotrophoblasts less numerous, and the stroma with more collagen. The fetal vessels become larger and more toward the periphery of the villus. In the third trimester, the villi are much smaller in diameter, and the cytotrophoblasts are irregular and thinned out. The fetal vessels are dilated and lie just below the thinned out trophoblasts.
The placenta, at term, is almost a circular disc with a diameter of 15–20 cm and a thickness of about 3 cm at its center [2]. It feels spongy and weighs about 500 g, the proportion to the weight of the baby being roughly 1:??6 at term and occupies about 30% of the uterine wall. It presents two surfaces, fetal and maternal, and a peripheral margin (Figure 3) [2].
The fetal surface is covered by the smooth and glistening amnion with the umbilical cord attached at or near its center [2].
The maternal surface is rough and spongy. It consists of 15–20 lobes or cotyledons which are limited by fissures. Each fissure is occupied by the decidual septum which is derived from the basal plate [2].
Figure 3.
Placenta at term.
The placenta consists of two plates. The chorionic plate lies internally. It is lined by the amniotic membrane. The umbilical cord is attached to this plate. The basal plate lies to the maternal aspect. Between the two plates lies the intervillous space containing the stem villi with their branches, the space being filled with maternal blood. A mature placenta has a volume of about 500 mL of blood, 350 mL being occupied in the villi system and 150 mL lying in the intervillous space [2].
3. Functions
Transfer of nutrients and waste products between the mother and the fetus. In this respect, it attributes to the following functions:
Respiratory
Excretory
Nutritive
Endocrine function: placenta is an endocrine gland. It produces both steroid and peptide hormones (like progesterone, estriol, human chorionic gonadotropin, and human placental lactogen) to maintain pregnancy and support fetal growth.
Barrier function: placenta acts as a protective mechanism.
Immunological function: maternal antibodies are taken into the syncytiotrophoblasts by pinocytosis and subsequently transferred to fetal capillaries and thus fetus acquires passive immunity (Figure 4).
Figure 4.
Blood supply of placenta.
4. Abnormalities of placenta
4.1. Placenta succenturiata
The accessory lobe is developed from the activated villi on the chorionic leave, may be placed at varying distances from the main placental margin. A leash of vessels connecting the main to the small lobe traverses through the membranes (Figure 5). In cases of absence of communicating blood vessels, it is called placenta spuria. The incidence of placenta succenturiata is about 3%. If the succenturiate lobe is retained, the following birth of the placenta may lead to:
Postpartum hemorrhage which may be primary or secondary
Subinvolution
Uterine sepsis
Polyp formation
Figure 5.
Placental abnormalities.
Treatment: Whenever the diagnosis of missing lobe is made, exploration of the uterus and removal of the lobe under general anesthesia is to be done.
4.2. Velamentous placenta
Normally, the umbilical cord inserts into the middle of the placenta as it develops. In velamentous cord insertion, the umbilical cord inserts into the fetal membranes (chorioamniotic membranes) and then travels within the membranes to the placenta (between the amnion and the chorion). The exposed vessels are not protected by Wharton's jelly and hence are vulnerable to rupture (Figure 5). Rupture is especially likely if the vessels are near the cervix, in which case they may rupture in early labor, likely resulting in a stillbirth. Once it is diagnosed, baby should be delivered by cesarean section.
4.3. Battledore placenta
Umbilical cord may be attached in the center, off center, on the edge, or in the membranes of the placenta. Battledore placenta is a placenta in which the umbilical cord is attached at the placental margin. The shortest distance between the cord insertion and the placental edge is within 2 cm. The incidence of the battledore placenta is 7–9% in singleton pregnancies and 24–33% in twin pregnancies [4, 5]. Complications associated with the battledore placenta are:
fetal distress
intrauterine growth restriction
preterm labor
decreased birth weight of baby and placenta
4.4. Placenta extrachorialis
It can be:
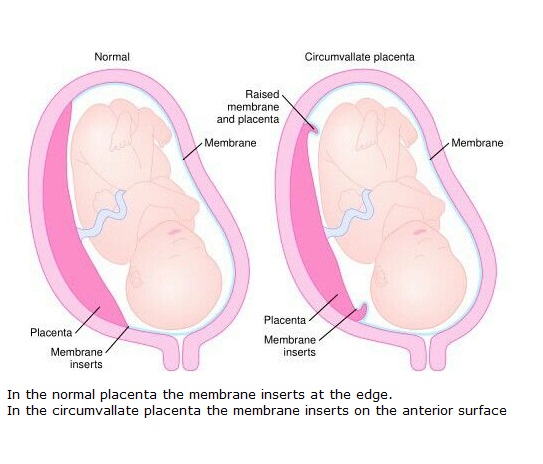
Circumvallate placenta: the fetal surface is divided into a central depressed zone surrounded by a thickened white ring which is usually complete. The ring is situated at varying distances from the margin of the placenta and is composed of a double fold of amnion and chorion with degenerated decidua (vera) and fibrin in between. Vessels radiate from the cord insertion as far as the ring and then disappear from view.
Placenta marginata: a thin fibrous ring is present at the margin of the chorionic plate where the fetal vessels appear to terminate.
There is increased chance of:
Abortion
Hydrorrhea gravidarum
Antepartum hemorrhage
Growth retardation of the baby
Preterm delivery
Retained placenta or membranes
4.5. Morbidly adherent placenta
Morbidly adherent placenta, which includes placenta accreta, increta, and percreta, implies an abnormal implantation of the placenta into the uterine wall (Figure 6). The incidence of placenta accreta has increased significantly over the past several decades, with the main risk factors including prior cesarean section and placental previa. Sonographic markers of placenta accreta can be present as early as the first trimester and include a low uterine implantation of a gestational sac, multiple vascular lacunae within the placenta, loss of the normal hypoechoic retroplacental zone, and abnormality of the uterine serosa-bladder interface, among others.
Placenta accreta is an extremely rare form in which the placenta is directly anchored to the myometrium partially or completely without any intervening decidua. The probable cause is due to the absence of decidua basalis and poor development of the fibrinoid layer.
Placenta increta: The placenta invades whole thickness of myometrium.
Placenta percreta: The placenta penetrates whole of the myometrium and may reach up to the peritoneum or bladder.
Figure 6.
Morbidly adherent placenta (A: Accrete, B: Increta, C: Percreta).
4.6. Gestational trophoblastic disease/neoplasm
Gestational trophoblastic disease is divided into molar and nonmolar tumors. Nonmolar tumors are grouped as gestational trophoblastic neoplasia. It is classified as:
Hydatidiform mole
Complete
Partial
Gestational trophoblastic neoplasia
Invasive mole
Choriocarcinoma
Placental site trophoblastic tumor
Epithelioid trophoblastic tumor
4.7. Chorioangioma of placenta
Placental chorioangioma is the commonest benign tumor of the placenta. Its incidence is around 1% when examined microscopically and is seen more frequently in multiple pregnancies and in female babies [6]. Chorioangiomas that are clinically evident are less common with an incidence between 1:3500 and 1:9000 births [6]. It is believed to arise by 16th day of fertilization, although there is no documentation of the tumor in the first trimester [7]. In the majority of cases, it is small or microscopic and of no clinical significance. If it increases in size >5 cm, then it may be associated with serious maternal and fetal complications (Figure 7) [6].
Figure 7.
Chorioangioma of placenta.
The pathogenesis of these neoplasms is controversial; however, they can originate from any part of the placenta excluding the trophoblastic tissues [8]. Three histological patterns of chorioangiomas have been described: angiomatous, cellular, and degenerate [9];
The angiomatous is the most common, with numerous small areas of endothelial tissue, capillaries, and blood vessels surrounded by placental stroma.
The cellular pattern has abundant endothelial cells within a loose stroma.
The degenerate pattern has calcification, necrosis, or hyalinization.
These lesions are sometimes classified as placental hamartomas rather than true neoplasia [10]. There is no malignant potential.
Large tumors probably act as arteriovenous shunts and cause complications. Maternal complications are preeclampsia, preterm labor, placental abruption, polyhydramnios, and postpartum hemorrhage [11]. The correlation of chorioangioma with hydramnios and preterm delivery is found to be significant among the various reported clinical complications. Fetal congestive heart failure may develop because of the increased blood flow through the low resistance vascular channels in the chorioangioma acting as an arteriovenous shunt. Other associated fetal complications are nonimmune hydrops, fetal demise, hemolytic anemia, congenital anomalies, fetal thrombocytopenia, cardiomegaly, intrauterine growth restriction, and neonatal death [12].
Antenatal ultrasound examination has made diagnosis and follow up possible before delivery. In the present case, the placental tumor was not diagnosed in the ultrasound documentation rather polyhydramnios was reported. Doppler ultrasound examination is the gold standard in primary diagnosis of hemangioma. But unfortunately, we could not conduct Doppler USG in the present case as delivery was imminent. Magnetic resonance imaging (MRI) is used only in suspicious cases, while the computed tomography (CT) technique has a limited role in the diagnosis of the placental angioma, mainly because of the high radiation risk and poor tissue differentiation.
Chorioangioma with complications before fetal viability requires interventions. Alcohol injection, laser coagulation of feeding vessels, and microcoil embolization of the feeding vessels are described for women with fetal complications like hydrops [13, 14]. Large chorioangioma associated with polyhydramnios leads to high perinatal morbidity and mortality. Polyhydramnios is treated with therapeutic amniocentesis and maternal indomethacin therapy [12]. Steroid administration for acceleration of fetal lung maturity before 34?weeks is indicated. If complications appear late in pregnancy, delivery is the choice. A recent literature review concluded that further studies are needed to refine the appropriate selection criteria that will justify the risk of invasive in utero therapy for chorioangiomas [15].